Breakthrough technology indicates earlier detection for Alzheimer’s disease
A research team co-led by a scientist at City University of Hong Kong (CityU) has discovered a new, non-invasive way to detect early-stage Alzheimer’s disease, helping patients get the necessary treatments around 10 years before any symptoms appear.
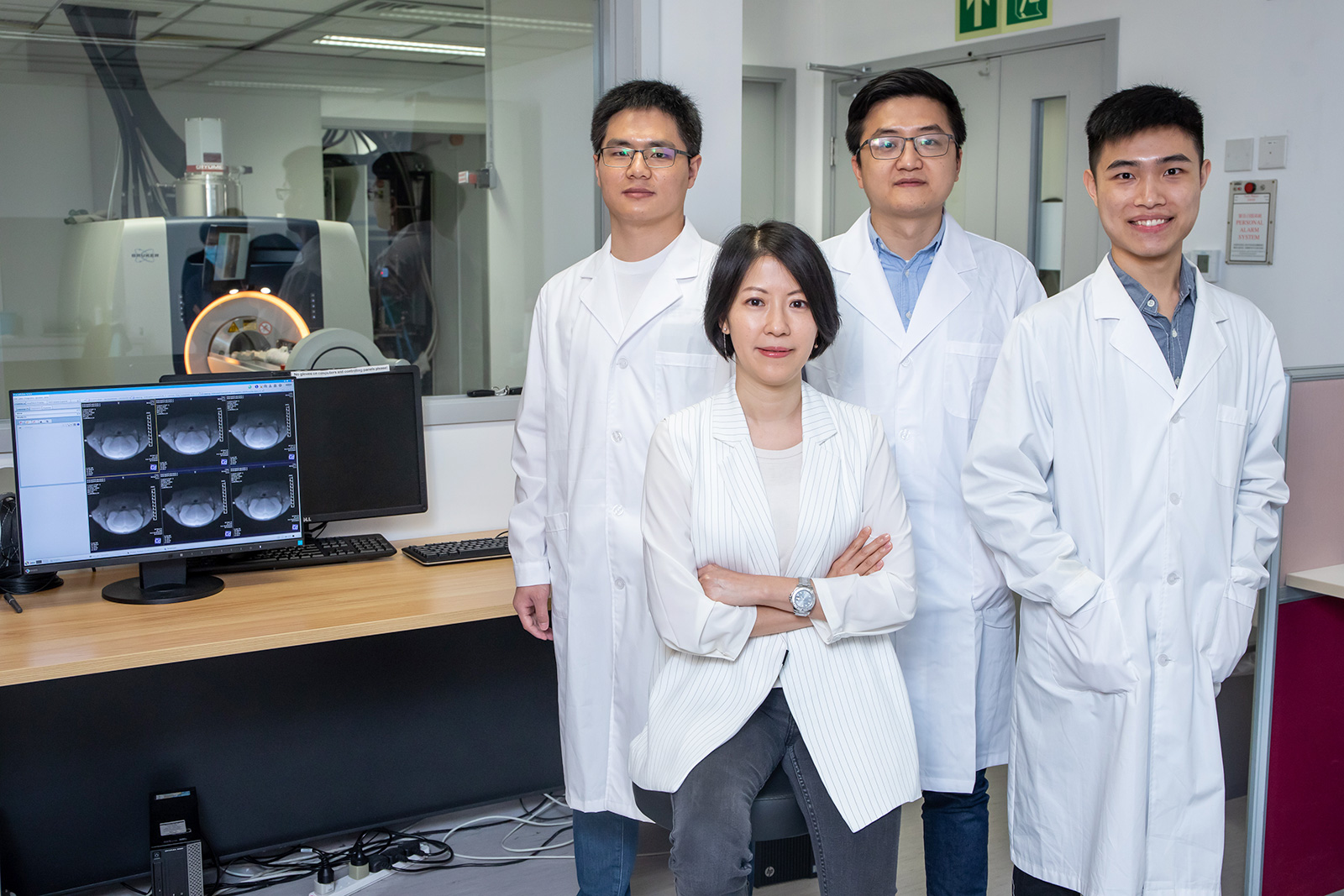
In collaboration with Johns Hopkins University in the US, Dr Kannie Chan Wai-yan, Associate Professor in the Department of Biomedical Engineering (BME) at CityU, and her research team have developed a molecular imaging approach based on Magnetic Resonance Imaging (MRI). The MRI approach dynamically measures changes in the levels of glucose in the brain’s lymphatic system, which could provide early clues about the disease.
According to Dr Chan, the tricky part in identifying Alzheimer’s disease is that early abnormalities such as the emergence of protein plaques are similar to the normal ageing process seen in the human brain. Even more challenging, symptoms might appear years after pathologies in the brain occur.
One of the hallmarks of early Alzheimer’s disease is glucose uptake and clearance in the glymphatic system, which is the lymphatic system in the brain. Currently, glucose uptake and metabolism can be assessed using positron emission tomography (PET) in hospitals. However, PET scans with radioactive tracers are expensive and its invasive nature has hindered its general clinical application. In addition, patients cannot be scanned too frequently with radioactive tracers.
Dr Chan’s team’s new imaging approach based on Chemical Exchange Saturation Transfer MRI (CEST MRI) assesses the glucose uptake and clearance in the lymphatic system in the brains of mice in a non-invasive way.
“While CEST MRI has been used in the diagnosis of brain tumours before, this is the first time it has been used in assessing the function of the lymphatic system,” said Dr Chan.
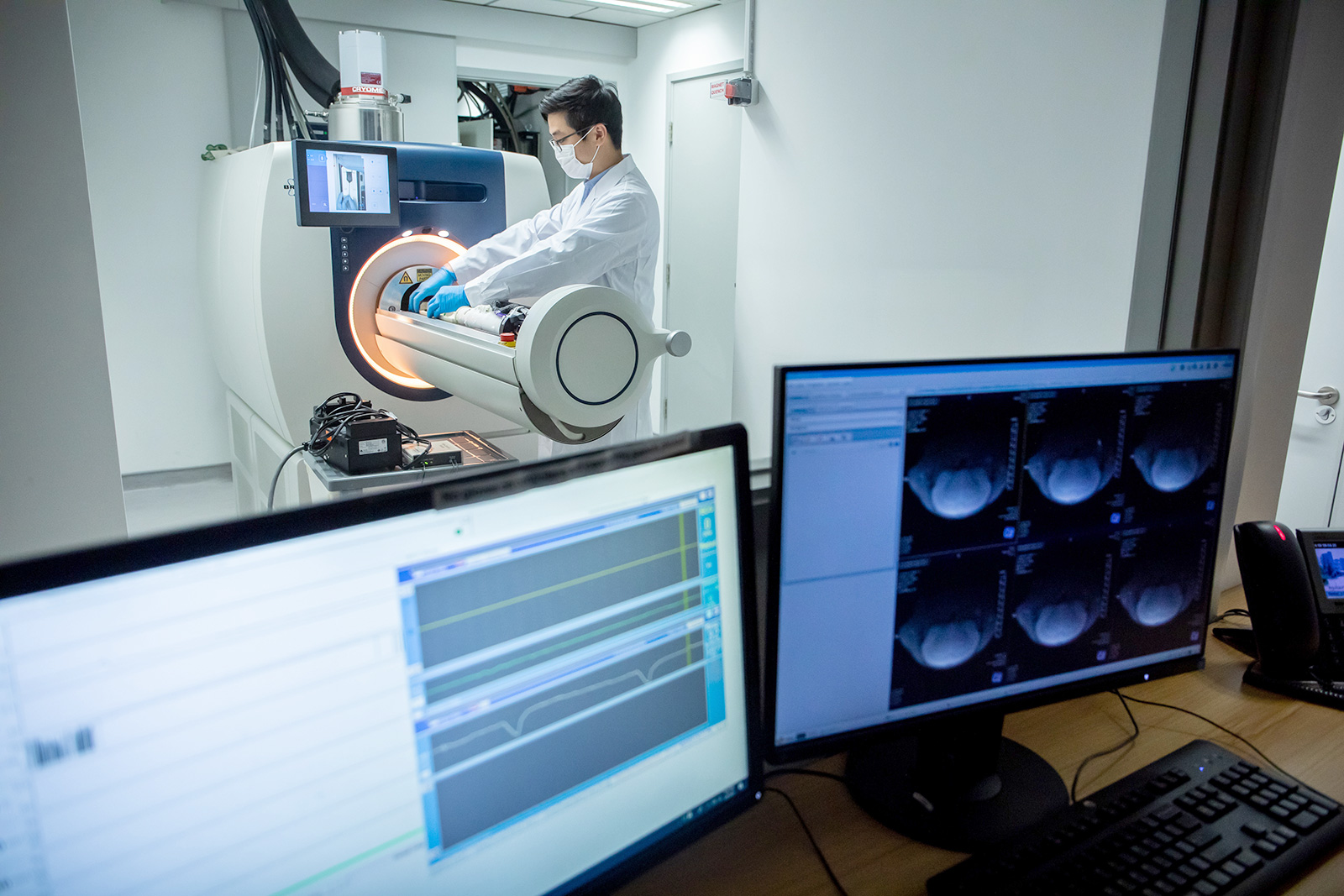
The team carried out the experiments using a 3T MRI animal scanner at CityU, the only one of its kind in Hong Kong. They injected glucose into the mice with Alzheimer’s disease and healthy mice aged 6 months and 16 months. The dynamic response of glucose both in the cerebrospinal fluid and brain parenchyma were then measured simultaneously using the CEST MRI.
According to MRI results, the team observed that mice with Alzheimer’s disease show significantly reduced clearance rates of cerebrospinal fluid compared to age-matched healthy mice due to abnormalities in the brain’s drainage system.
Moreover, a significantly higher glucose uptake was detected in the brain parenchyma of the six-month-old mice with Alzheimer’s disease compared to healthy mice of the same age. For the 16-month-old mice with Alzheimer’s disease, a significantly lower glucose uptake was found in both the brain parenchyma and the cerebrospinal fluid compared to the healthy mice.
These results echo previous research findings using other methodologies and serve as benchmarks for distinguishing Alzheimer’s disease from normal ageing. Importantly, abnormalities are detected at the early stage of Alzheimer’s disease when little neuropathology has developed in the brain, thus contributing to halting or at least slowing down progression into a more devastating stage of the disease that affects the daily life of patients.
“By using glucose as a ‘tracer’, our imaging method can sensitively detect distinctive changes in the lymphatic system function at the molecular level at an early stage of the disease, helping us to differentiate from normal ageing,” said Dr Chan.
The team believes this non-invasive assessment of the glymphatic system can serve as an imaging biomarker to reveal early pathology of Alzheimer’s disease.
“Glucose is natural, biodegradable and commonly used in hospitals for tests such as glucose tolerance. Using it as a contrast agent for MRI is non-invasive and safe,” she added.
The new imaging method is compatible with MRI machines commonly-used in clinics and hospitals, which means a low set-up cost and an easier transfer to clinical applications. Dr Chan anticipates that clinical trials can be conducted in three years.
The findings were published in the latest issue of the scientific journal Science Advances under the title “Altered D-glucose in brain parenchyma and cerebrospinal fluid of early Alzheimer’s disease detected by dynamic glucose enhanced MRI”.
Dr Chan and Dr Xu Jiadi from Johns Hopkins University School of Medicine are the corresponding authors of the paper. The first author of the paper is Huang Jianpan, PhD student from CityU’s BME. Other co-authors from CityU included Han Xiongqi and Joseph Lai Ho-chi, PhD students from BME. Research team members also included Professor Peter C. M. van Zijl from Johns Hopkins University, Professor Wu Xuekui from The University of Hong Kong, and Professor Linda Knutsson from Lund University.